The GP or an Emergency Department are likely to be the first medical professionals you engage with after developing a facial palsy and many people will not be routinely followed up. This information aims to help you understand when to seek a referral for specialist help for facial palsy via your GP.
If you have facial palsy due to surgery, trauma or tumour removal, you should already be engaging with consultants at the hospital. If you have been discharged from hospital but still need further help, you can also refer to this information for how to approach your GP.
Children born with facial palsy are often reviewed in childhood but may not have been followed up properly in adulthood, this is another reason why someone may want to seek further help.
Where a diagnosis has been made of Bell’s palsy or Ramsay Hunt syndrome the treatment is usually medication with around three quarters of people making a full recovery without further intervention. Your health care provider should have ruled out other causes of the facial palsy at this point or if in any doubt arranged for further investigations.
Below we explain the normal treatment given for the more common acquired conditions – Bell’s palsy and Ramsay Hunt syndrome. We also explain when and how to seek help for other causes of facial palsy.
Quick links to sections in this article:
- Bell’s palsy
- Ramsay Hunt syndrome
- When to seek help for facial palsy
- Why don’t GPs immediately refer patients to a specialist?
- My GP says I must wait at least six months to a year before I can have a referral, is this correct?
- Why do I need to see a specialist facial therapist?
- Why do we recommend patients are managed by a multidisciplinary team where possible?
- Long term facial palsy due to any cause
- Approaching your GP
- Preparing for your appointment with a specialist
- Preparing for your appointment for Botulinum Toxin injections
Bell’s palsy
The normal treatment for Bell’s palsy is steroids (within 72 hours of initial symptoms) and preservative free eye ointment and/or drops. Those newly diagnosed often feel they should be doing something extra to help their recovery such as facial exercises. Without guidance from a medical expert these can actually do more harm than good when the muscles are weak, floppy and immobile (flaccid stage). The best thing to do is rest at this stage and give the nerve time to recover, although facial massage is recommended. You can still make your normal facial movements, just don’t try and force exaggerated movements. You want your face to recover to its natural state and doing forceful movements is unnatural. There are a set of videos on the Facial Palsy UK website which detail safe interventions to do during the flaccid stage.
Link to flaccid paralysis self-help videos
Report any of the following symptoms to your GP:
- If your face is extremely painful and keeping you awake at night.
- Any rash in or around the ear, in the hairline, or sores in the mouth.
- If you have recently been bitten or notice a bull’s eye shape rash anywhere on your body.
- Any balance issues/vertigo.
- Any hearing loss or tinnitus.
- Any weakness in one side of your body or cognitive difficulties (difficulty thinking and/or organising your thoughts).
- Any facial swelling, or folds or furrows in the tongue.
Usually doctors are very good at ruling out other causes but occasionally they are missed, particularly Ramsay Hunt syndrome which is much more painful than Bell’s palsy, as it is a shingles viral infection.
Women in the last trimester of pregnancy are at a higher risk of developing Bell’s palsy than the general population. Corticosteroids are considered safe for the management of many medical conditions during pregnancy, so this option should always be considered by a health professional aware of the patient’s complete medical history. You can find out more information about facial paralysis in pregnancy here.
Link to facial paralysis in pregnancy
Ramsay Hunt syndrome

Mnemonic – spot the warning signs of Ramsay Hunt syndrome
The normal treatment for Ramsay Hunt syndrome is steroids and antivirals both to be given within 72 hours. You should also speak to your doctor about pain relief, preservative-free eye ointment and/or drops. As with Bell’s palsy, we do not recommend trying to do facial exercises during the early stages of your recovery, but you can follow this set of videos on the Facial Palsy UK website for safe self-help tips.
Link to flaccid paralysis self-help videos
When to seek help for facial palsy
Eye health
If your eye does not close properly after 2-3 weeks you should be referred to ophthalmology as prolonged drying of the eye can lead to permanent damage. If your eye is watering profusely it is often a sign it is too dry, and you need to use more eye lubricant, it tends to overwater to compensate for the dryness.
In the later stages of recovery some people develop crocodile tears where the eye waters involuntarily, particularly whilst eating. This is due to faulty ‘re-wiring’ of the nerves during the recovery phase and is a separate complication that you would discuss with a facial palsy specialist consultant or ophthalmic consultant.
General facial recovery
Seek a referral to a facial nerve specialist if there is any doubt about the diagnosis, or you have had:
- No improvement at all after three weeks of treatment.
- Incomplete recovery three months after onset of initial symptoms.
Many people assume that the specialist they need to see is a neurologist when in fact a facial nerve specialist could be a plastic surgeon, ENT consultant or neurologist. In some cases, you might be referred directly to a specialist facial therapist. There are very few facial nerve specialists in the UK, if your GP is unsure where to refer they can contact Facial Palsy UK.
If you have not made a full recovery after three months and are waiting for a referral it may be appropriate for you to follow our guidance on ‘paresis stage exercises’. You should only do these if you fulfil all of the three criteria below:
- Your face is more symmetrical at rest.
- Your facial muscles have more shape and springiness and are no longer floppy.
- You have noticed some small flickers of movement when you make facial expressions.
If there is clear evidence of these three signs then your face is no longer flaccid. It means you have reached the paretic stage of recovery and it is safe to carry out our paresis stage exercises. This is good news but also a point at which you should exercise great caution. Any forceful exercising will encourage the development of involuntary movements (synkinesis) so all movement exercises should be done using:
- Very low effort/force.
- All movements should be slow, gentle and symmetrical.
- Never practise asymmetrical movements.
It is very important that you read the guidance carefully to make sure these exercises are suitable for you and watch the videos at least every week to ensure you are carrying out the exercises accurately.
Very important! – If you have undergone dynamic or static surgery to restore facial symmetry and/or movement you should not do the paresis stage exercises. You should follow the guidance given by your surgeon or clinician in charge of your care.
Why don’t GPs refer patients immediately to a specialist?
This is often because many people with Bell’s palsy or Ramsay Hunt syndrome will make a full recovery with no further intervention necessary. A GP would be more likely to refer a patient if there was uncertainty about their diagnosis and they needed further investigations such as an MRI or CT scan.
My GP says I must wait at least six months to a year before I can have a referral, is this correct?
Unfortunately, once stroke is ruled out, referral pathways are inadequate or missing for facial palsy in many areas of the UK, Facial Palsy UK is trying to improve this situation. This can lead to people waiting months or in some cases years for an appropriate referral. If you have an incomplete recovery it is much better to see a specialist as soon as possible. You can read about the stages of recovery here:
A specialist facial therapist can give you bespoke facial exercises to do and as everyone’s face is different you will need expert guidance. Synkinesis is a long-term side effect when people do not have a complete recovery from Bell’s palsy. In a prolonged recovery, the facial nerve can send messages to the wrong facial muscles creating unwanted linked movements, e.g. your eye closes every time you smile. Delaying a referral to a facial therapist can make these incorrect movements much more difficult to put right, as facial muscles can soon learn incorrect patterns of behaviour. The goal here is prevention and to minimise the amount of facial retraining required. Delaying the referral could be costlier to the NHS in the longer term as more interventions may be needed.
My GP wants to know why I need to see a specialist facial therapist and not a general physiotherapist, what is the difference?
Understanding and management of facial palsy which is not caused by a stroke has seen a dramatic improvement in the last 10 – 15 years. This is due to practicing clinicians, particularly plastic surgeons, physiotherapists and speech and language therapists, taking a special interest in how the facial nerve recovers following injury to the nerve itself and how therapy and/or surgery can maximise a person’s potential to recover. However, this wealth of information is not yet part of the curriculum for trainee physiotherapists and speech and language therapists. The majority of therapists graduating will have learned about the treatment for facial palsy following a stroke. This is a very important distinction, as the recovery for those with stroke (damage to the cortex of the brain), and the recovery for those with an injury to the facial nerve is very different. As a result, most therapists will have a good understanding of stroke rehabilitation but little or no understanding of rehabilitation following facial nerve injury. The following link provides a comprehensive list of the possible causes of facial nerve injury.
There are some fundamental differences in the management of facial palsy which require a completely different approach. Further information will be made available on our dedicated health professionals website when it launches.
Why do we recommend you are referred to a multidisciplinary team (MDT)?
A facial palsy multidisciplinary team normally includes different specialist consultants and a specialist facial therapist providing diagnosis, surgical options, management of eye health, and specialist facial therapy. In an ideal world we would also like to see psychology routinely offered as part of the MDT but there are currently only a handful of clinics in the UK offering this additional support. Often when funds are cut some of the wider services such as psychology are only offered to patients who have had surgery. We are working to raise awareness and improve this situation. Some hospitals are also cutting access to specialist facial therapy with little understanding of the potential longer term cost savings to the NHS.
Some patients receive treatment from a specialist surgeon experienced in treating people with facial palsy. Treatment usually involves injections of Botulinum Toxin (BT), commonly referred to as ®Botox, for problems with muscle contractures (thickened and shortened facial muscles), synkinesis (involuntary facial movements/spasms), and contra-lateral dominance (dominance of the unaffected side). However, these patients do not receive specialist facial therapy as part of their wider treatment plan. BT is a short-term solution to managing contracted facial muscles and involuntary (synkinetic) movements because it generally wears off in 3 to 5 months. While the muscles are relaxed following injections of BT, it is easier and less painful for patients to do facial rehabilitation exercises. Guided by a specialist facial therapist, the patient can practice muscle releases (stretches) to permanently lengthen muscles which have become short, tight and immobile, as a relaxed muscle is easier to lengthen than one which is tight. The process of lengthening is very slow but enhanced by the use of BT injections. Therapists also carry out neuro-muscular retraining (NMR) exercises to aid inhibition of synkinesis and promote the development of normal facial movement. NMR exercises are difficult to perform correctly without the help of BT because synkinesis occurs in tandem with voluntary movements. These exercises are easier for patients to perform after treatment with BT because the injected muscles are weaker and less able to make these unwanted, simultaneous synkinetic movements. BT can therefore help with the correct repatterning of facial movements. BT should be seen as an adjunct to therapy by providing a window of opportunity for effective exercising. This will help facilitate permanent lengthening and mobility of the facial muscles and correct movement patterns. If a patient only receives BT but does not work on building length back into the muscles and inhibiting synkinesis, once the Botox wears off the patient will lose all the benefit they gained.
It is also important to see what can be achieved by specialist facial therapy before considering invasive surgeries. By different team members of the MDT working together, they optimise the care for the patient.
There are some specialist multidisciplinary teams in England and Scotland although patients often find they have to travel long distances for appointments.
The Welsh situation: a new facial palsy service has launched in Wales at the Morriston Hospital in Swansea but the clinic lead (a plastic surgeon) is not currently supported by a specialist facial therapist but we are working to improve this situation. People in North Wales are able to access the multidisciplinary team based at Whiston Hospital in Prescot, part of St Helens and Knowsley Teaching Hospitals. Facial Palsy UK will be funding training for specialist facial therapy in Wales but it is important that a therapist is part of a clinic where they will see a good number of patients with facial palsy otherwise these skills will not be developed and honed by clinical practice.
The Northern Irish situation: there is a team of health professionals in Belfast who want to set up a dedicated facial palsy clinic but unfortunately the service is not currently funded. Some patients are accessing Botox injections, facial therapy and psychological support as part of other clinics but a properly funded multidisciplinary approach is needed. It is important that a facial therapist is part of a clinic where they will see a good number of patients with facial palsy otherwise these skills will not be developed and honed by clinical practice.
Long-term facial palsy due to any cause
People often ask whether it is too late to seek help if they first had a facial palsy, for example, more than twenty years ago. There are more than fifty different causes of facial palsy and it is common for people to go years without any support. There are many ways that symptoms can be improved resulting in a better quality of life. There is no cure for a facial nerve that is permanently damaged but with the right expertise there are ways to reduce facial tightness and pain, involuntary movements, etc. Surgeries will never restore a face to what it once was but can help to improve symmetry and improve the smile in some patients. It is never too late to seek help.
If you have long-term facial palsy and are suffering with tightness in the face you can follow the videos on this page while you wait for your referral.
Important! – If the tightness is due to surgery please speak to a specialist facial therapist before undertaking facial exercise.
You may have been born with facial palsy and have started having more problems as your face ages, e.g. the face may droop more on the paralysed side pulling the lower eyelid down causing more dry eye than you experienced previously. There is help available, particularly if your vision is at risk.
Approaching your GP
There is a lack of awareness about the impact of facial palsy among many health professionals. This means it is really important to describe all of the functional issues that are affecting your daily life when approaching your GP. They won’t necessarily know much about the long-term effects of facial palsy, so you should not assume they do.
With pressures on the NHS for funds it is important your GP realises this is not cosmetic otherwise they may refuse to refer you.
Before you approach your GP make a list of the functional and psychological ways your facial palsy affects you. You may just have accepted that things will not change and omit to tell your GP certain issues. It is really important you tell them everything.
Tell them about:
- Facial pain or tightness, including headaches.
- Involuntary movements, e.g. if your eye closes when you smile, if your cheek lifts unexpectedly.
- Problems with vision, if your eye closes unexpectedly or is too dry or over-waters, or if you have poor eye closure.
- Any neck spasms or cramps (this is often related to acquired facial palsy).
- Any dental issues, dry mouth or eating difficulties.
- Speech difficulties and if it is tiring to speak for too long.
- How it psychologically affects you, if you have adapted your life because of facial palsy, e.g. stopped going out so much.
You need to provide lots of detail because if you only tell your GP you don’t like your face or how your face looks, they may dismiss the condition as cosmetic. We obviously know that facial palsy is much more complicated than that, but you will have to educate them because many will not know enough about the impact of facial palsy. Your GP needs to understand that it is not just about what they see, it is about how you feel and if you are constantly distracted and reminded by twitches and tightness in your face make sure they understand this. If it is easier than verbally explaining why you want to see a specialist, you could give a written list to your GP and say this is what you need help with. If your GP refuses to refer you, ask them to put in writing the reason for their refusal.
Often it can help if you know where you want to be referred to. If your GP refuses to refer you to the specialist of your choice and this is your first outpatient appointment for facial palsy, please note that in England patients have certain legal rights regarding the NHS known as Patient Choice. You can find out more information in the link below.
NHS – choosing a hospital or consultant
If your GP refuses your referral due to lack of funding, refer to the following page for more help or contact us for further support.
Preparing for your appointment with a specialist
If you are able it may be useful to do the following:
- Find a photograph of yourself before you had your facial palsy and take it to your first appointment. This will give the clinician a good baseline to work towards and enable them to assess your degree of facial symmetry prior to your facial palsy. It is important to understand that faces are never completely symmetrical and natural asymmetries may become more apparent as we age.
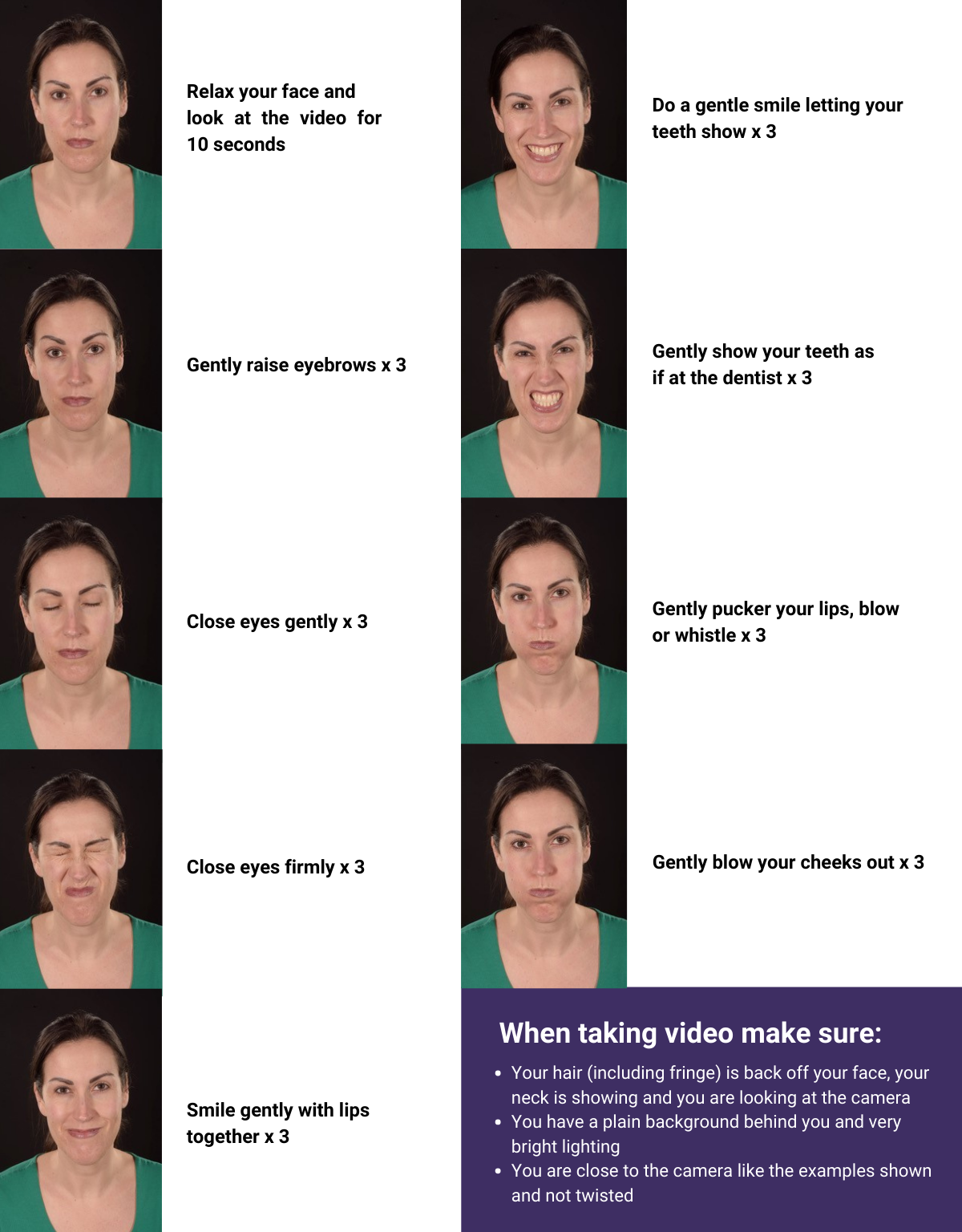
- If you have kept a photographic log of your recovery please take these to your appointment so the clinician can see how you have progressed. If you are waiting for your referral/appointment then start recording your progress while you wait by taking photographs or preferably a video of yourself every four weeks or more frequently if you have noticed a specific change. Include the following expressions but do them as gently as possible:
- Look surprised
- Close your eyes
- Smile
- Snarl
- Whistle
- Blow your cheeks out
Preparing for your appointment for Botulinum Toxin injections
The information below is specifically designed for people who are attending appointments for Botulinum Toxin injections.
If subsequent appointments include treatment with Botulinum Toxin injections then take the same photographs and videos before your treatment. Repeat these two weeks later so that you can see how effective the treatment has been. Take these to your next appointment for repeat injections to show your clinician. This will enable him/her to adjust the dose accordingly and or increase/decrease the number of injection sites.
See examples below of facial expressions to record, preferably with video.
For more information about Botulinum toxin and its use for treating facial palsy please visit our dedicated webpage (link below).
If you need any further help please contact our support team.
FPUK Associated Articles:
Last reviewed: 16-10-2023 || Next review due: 16-10-2025
